December 2018 - NON-MEDICATED LIFE
Preventing and Treating Gout
By Dr. Paul E. Lemanski, MD, MS, FACP
Medicines are a mainstay of American life and the healthcare system not only because they are perceived to work by the individuals taking them, but also because their benefit may be shown by the objective assessment of scientific study. Clinical research trials have shown that some of the medicines of Western science may reduce the risk of heart attacks, strokes and cardiovascular death, while others may reduce certain types of cancer.
In the first 85 installments of the Non-Medicated Life, informed diet and lifestyle have been shown to accomplish naturally for the majority of individuals, many, if not most of the benefits of medications in the prevention and treatment of chronic medical conditions. Moreover, as a medical intervention they may accomplish such benefits with fewer side effects, may reduce the number and amount of medication, and may allow actual discontinuation of medication. This is true in the prevention and treatment of gout.
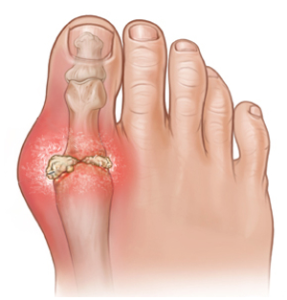
Gout is a condition caused by an increase in uric acid in the blood leading to the deposition of uric acid crystals in joints, kidney, skin and bones. In joints the uric acid crystals may cause inflammation of the joint with swelling, redness and severe pain. In those with such inflammation involving the big toe, called podagra, the pain can be so severe that the weight of the top sheet resting on the toe becomes unbearable. In those with persistently elevated uric acid, crystals may form a discreet mass-like collection called a tophus. When a tophus involves the joint, then bony destruction may ensue. When it involves the kidney, this collection may cause a kidney stone. And, when it involves the skin, it may appear as yellowish-white chalky nodules in the center of an area of localized redness and swelling.
Gout requires a genetic predisposition to either overproduce uric acid or an inability of the kidneys to efficiently excrete uric acid. As a consequence, uric acid builds up in the bloodstream causing a condition called hyperuricemia. Individuals may have hyperurecemia but not of a sufficient degree to cause the precipitation of uric acid crystals and a symptom. In most individuals an additional factor involving diet and/or lifestyle or medication is needed.
Diets high in purines are associated with gout. Purines are contained in most foods but are particularly high in meat and fish. Since the time of Hippocrates, gout has been associated with the consumption of meat and fish, and was referred to as “the disease of kings” because it appeared more prevalent in those wealthy enough to afford such food in excess. Additionally, gout is more prevalent in those who are overweight or obese and in those who consume alcohol to excess. Finally, gout is more prevalent in those who take certain types of diuretics.
In order to prevent gout, it is useful to know the risk factors for hyperuricemia and gout. The presence of hypertension, chronic kidney disease, cardiovascular disease, or metabolic syndrome (pre-diabetes) increases risk. The presence of an increased body weight, a diet high in meats, fish and alcohol, and a family history of gout may also increase risk. The more numerous the risk factors the greater the risk. Multiple risk factor individuals may want to consider a blood test to measure uric acid and should discuss this with their primary care physician. The presence of unexplained joint swelling, redness, and pain in a multiple risk factor individual should certainly prompt such a discussion.
If uric acid is elevated in an asymptomatic individual lifestyle, dietary and medication changes may help prevent the development of a new case of symptomatic gout. Once gout is established such changes may help but may not be sufficient to avoid medication. The exceptions to this include the intervention of weight loss in those overweight and obese, the avoidance of sugar sweetened beverages, the moderation of alcohol intake, and the use of whole diet approaches such as the DASH diet. These interventions seem to work both in preventing new cases of gout and reducing the symptoms and flares in those with established gout.
In a 12-year study of 47,000 health professionals, the risk of new onset gout was higher in those with a BMI >/= 25 (overweight) with the risk rising with BMI. In a prospective trial involving 4,000 obese patients without a history of gout undergoing bariatric surgery (compared to a control group treated non-surgically), bariatric surgery resulted in a 17% lower BMI (with the BMI of the control group increasing by 2%), and a statistically significant reduction in new onset gout compared to control. In a study of 99 morbidly obese patients with established gout, flares of gout were higher in the first post-operative month, but then decreased from 24% to 8% during months one to 13.
With regard to alcohol consumption, the risk of new gout was increased with the use of beer or liquor, but not wine. Compared to no beer intake, drinking two or more beers a day increased the risk for new onset gout 2.5 fold. However, eight ounces of wine did not increase the risk of new cases of gout. By contrast, beer, liquor and wine increased the risk of a flare of gout equally in those with a history of gout.
Dietary composition, specifically increased meat and seafood, increases the risk of new cases of gout, but in clinical trials does not seem to have adverse impact on patients with established gout, despite the recommendation of published guidelines to reduce their consumption. Low-fat dairy has been shown to decrease new cases of gout but not exacerbations of those with a history of gout. Finally, whole food (predominately plant-based) diets like the DASH diet that emphasize fruits, vegetables and low-fat dairy with a reduction in high saturated fat containing meat, reduce new cases of gout as well as flares in those with established gout.
In summary, diet and lifestyle may help to prevent new cases of gout, and may help in the treatment of those with established gout. Specifically, weight loss in those overweight or obese, the avoidance of sugar sweetened drinks, moderation of alcohol intake, and the use of whole diet approaches that emphasize a predominately plant-based diet have been shown to be of greatest benefit. Utilizing such interventions may allow the prevention of gout in those at risk and reduce the need for medication in those with established disease.
Paul E. Lemanski, MD, MS, FACP (plemanski@capcare.com) is a board certified internist at Center for Preventive Medicine at Community Care Physicians in Albany. He is medical director of the Dept. of Community Medicine and Population Health at Community Care Physicians. Paul has a master’s degree in human nutrition, he’s an assistant clinical professor of medicine at Albany Medical College, and a fellow of the American College of Physicians.